Brain Health – What’s Flu Got to Do With It?
Corona and influenza viruses affect not only our lungs, but also our brain, possibly with long-term consequences.
Within the last hundred years, novel strains of corona and influenza viruses have caused several global pandemics. Their primary place of action is the respiratory tract, yet, already since the famous pandemic known as the Spanish flu (1918-1920), associated neurological complications have been reported. The symptoms range from mild cognitive deficits to encephalopathy, epilepsy, and dementia.
In the recent COVID-19 outbreak, patients frequently suffer from headache, dizziness, nausea, or decreased sense of smell and taste, suggesting that SARS-CoV2 may indeed affect the central nervous system (CNS). This is also visible for symptoms of Long-Covid, a term to describe the effects of Covid-19 that continue for weeks or months beyond the initial infection. Attention and memory disturbances obviously point towards associated neuronal dysfunction, even with moderate symptoms.
We are just beginning to understand the potential association between respiratory viral infections and chronic neurodegenerative diseases – in particular with a diffused state of consciousness known as delirium, which is associated with intensive care patients of Covid-19 and correlated in general to a doubling of the risk to be affected by Alzheimer’s Disease in later life.
Because of the time delay that may occur between the actual infection and the subsequent development of pathology, the direct nature of this connection will be difficult to elucidate in humans. Coming back to the example of the Spanish flu, patients developed neurological symptoms such as parkinsonism sometimes decades later. Therefore, we need animal models on which we base our hypotheses.
How Viruses Attack the Brain
It is noteworthy that some respiratory viruses can directly invade the brain (termed neurotropic) sometimes causing neuroinflammation. However, viruses blocked by the blood-brain barrier (non-neurotropic) can also trigger what is called a cytokine storm. This is an overshooting immune reaction with devastating effects on almost all organs of the body including the brain.
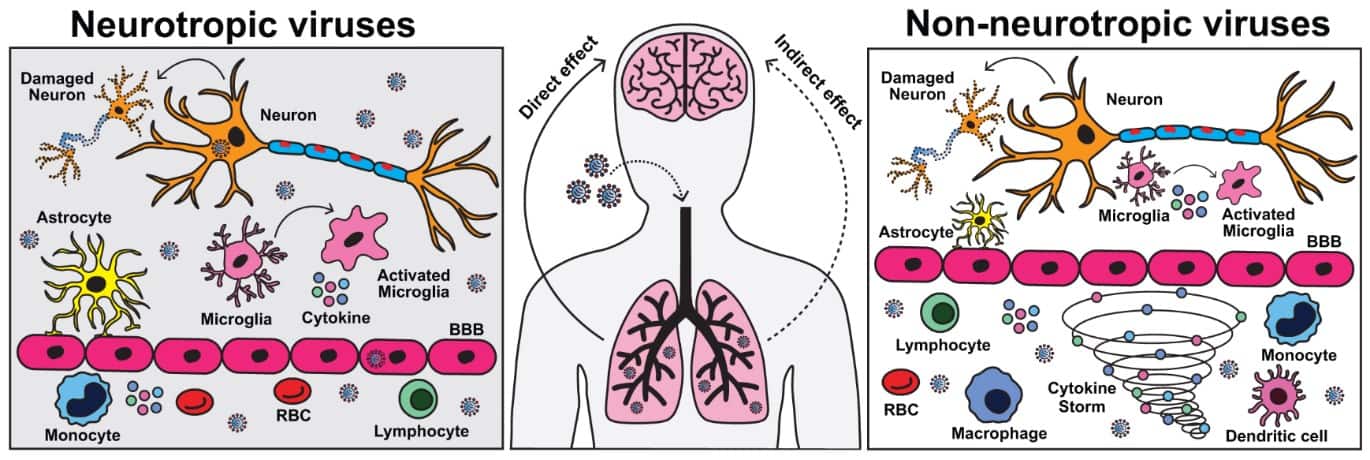
We recently published that a highly pathogenic influenza virus strain, such as H7N7 (avian influenza), can invade the brain during infection and cause direct neuronal damage and chronic activation of microglia cells, the immune cells of the brain. Yet, the strains most commonly isolated during seasonal influenza outbreaks (H1N1/H3N2) do not infect the brain but still are able to cause long-lasting chronic cognitive deficits – in particular in elderly individuals.
This emphasizes that the direct presence of a virus in the brain is not even necessary for neurological complications to occur. Even more that these manifestations might take much longer to recover than the acute symptoms of the initial infection.
Future Pandemics
Environmental and climate changes are predicted to enhance the frequency of new viral strains with pandemic potential, which also pose a possible threat to our most important organ, the brain. Strategies are needed not only to acutely fight viral infections but moreover to protect in particularly highly vulnerable brains with very limited regenerative capacity.
Thus, previous pandemics have taught us important lessons about what needs to be considered in future pandemics. We need to understand how immediate and delayed neurological damage is induced by different respiratory viral strains and how this might trigger or enhance neurodegenerative diseases.
This knowledge is crucial in order to treat symptoms or best of all prevent this downward spiral in the first place via vaccination or specific drugs, especially in vulnerable individuals such as the elderly.
Learn more in this related manuscript
[Title Image via Getty Images]
